
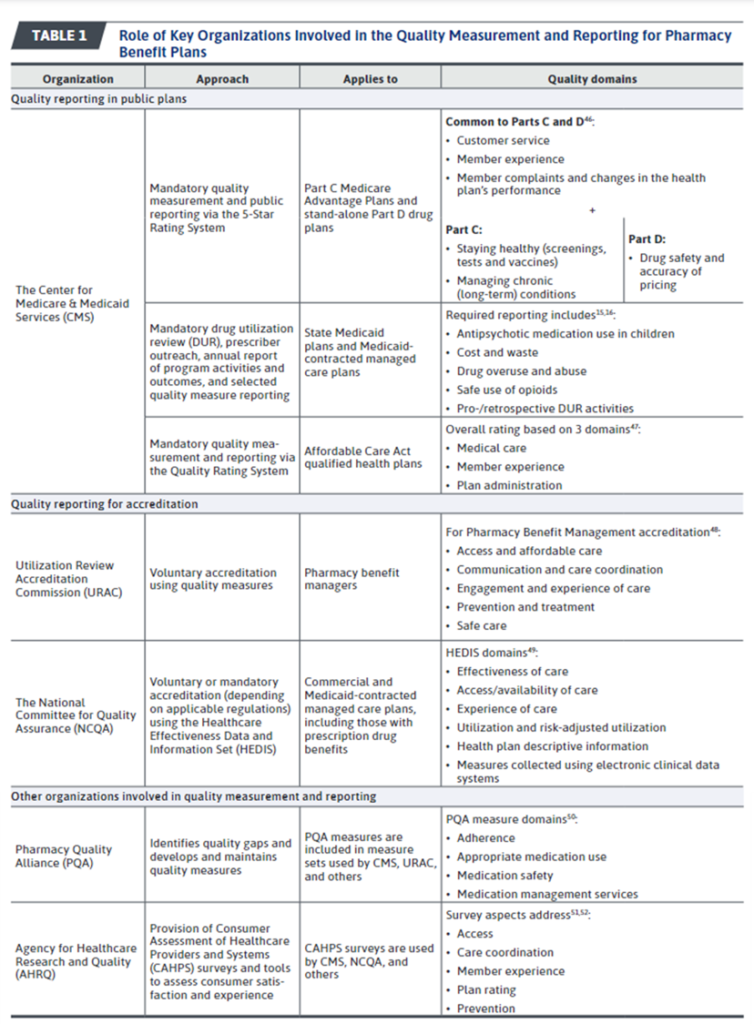
an article of Kogut (2024) has a good overview of organizations that develop pharmacy plan quality metrics. The quality of pharmacy plans is vital as approximately 85% of the US population has prescription drug coverage through public (e.g., Medicare, Medicaid) or commercial (e.g., employer-provided) pharmacy plans. . Below you will find a useful summary table.
Quality measures are selected based on evidence of validity (to ensure that the measure accurately represents the aspect of quality it is intended to measure), reliability (to ensure that the measure is accurate and estimation is done consistently), importance (i.e., aligns with key plan/population health priorities, usability (i.e., whether the metric is easily understood), feasibility (the burden imposed by the data collection necessary to estimate the measure), and consistency ( if it is consistent with other quality measures of another organization and does not duplicate other quality measures).
Of note is recent legislation affecting the measurement of quality of Medicaid plans.
The Substance Use Disorder Prevention Promoting Recovery and Opioid Treatment for Patients and Communities (SUPPORT) Act of 2018 introduced new requirements for state Medicaid DUR [drug utilization review] Medicaid-contracted managed care plans and programs. These requirements are designed to encourage the safe, effective, and efficient utilization of prescription opioids, with a focus on curbing overuse and misuse. Specific quality measurement topics include monitoring concurrent use of prescription opioids with benzodiazepines or antipsychotics, ensuring appropriate opioid dosing and limiting daily supply, and identifying cases of suspected abuse. Additionally, the SUPPORT Act mandated that Medicaid DUR programs monitor the use of antipsychotic medications in children.
One organization that experts in general (i.e., non-pharmaceutical) quality measures may be less familiar with is the Utilization Review Accreditation Commission (URAC).
URAC is the exclusive accreditation provider for pharmacy benefit management (PBM) companies offering pharmacy benefit plans. Although URAC accreditation is voluntary, URAC-accredited PBMs account for more than 90% of prescription drug volume in the United States.
More details on quality measurement, including how quality measurement attribution is determined and how medication therapy management (MTM) is implemented, are available in the full article. here.







